Notifiable Conditions
Healthcare Providers & Facilities
Notifiable to the local health jurisdiction (LHJ) of the patient’s residence unless otherwise designated
Download the Report ReferenceLegend
Immediately Notifiable
Requires a phone call to reach a live person at the local health jurisdiction, 24/7. Must be reported as soon as clinically suspected.
- Amebic meningitis
- Botulism, foodborne, infant, and wound
-
Coronavirus infection (severe communicable)
- SARS-associated coronavirus
- Novel coronavirus (COVID-19)
- Diphtheria
- Domoic acid poisoning
- E. coli (See “Shiga toxin-producing E. coli”)
- Influenza, novel or unsubtypable strain
- Measles (Rubeola) - Acute disease only
- Meningococcal disease, invasive
- Monkeypox (Mpox)
- Outbreaks and suspected outbreaks
- Paralytic shellfish poisoning
- Plague
- Poliomyelitis
- Rabies, suspected human exposure (suspected human rabies exposures due to a bite from or other exposure to an animal that is suspected of being infected with rabies)
- Rubella, acute disease only (including congenital rubella syndrome)
- Smallpox
- Tularemia
- Vaccinia transmission
- Viral hemorrhagic fever
- Yellow fever
Notifiable Within 24 Hours
Requires a phone call if reporting after normal public health business hours.
- Baylisascariasis
- Brucellosis
- Candida auris infection or colonization
- Hantaviral infection
- Legionellosis
- Leptospirosis
- Listeriosis
- Mumps, acute disease only
- Pertussis
- Psittacosis
- Q Fever
- Salmonellosis
- Shigellosis
- Tuberculosis disease (confirmed or highly suspicious, i.e., initiation of empiric treatment)
- Yersiniosis
- Unexplained critical illness or death
Notifiable Within 3 Business Days
- Acquired immunodeficiency syndrome (AIDS) Notifiable to: DOH (for facilities) and LHJ (for providers)
- Anaplasmosis
-
Arboviral disease (acute disease only) including, but not limited to:
- Chikungunya
- Dengue Eastern and western equine encephalitis
- Japanese encephalitis
- La Crosse encephalitis
- Powassan virus infection
- St. Louis encephalitis
- West Nile virus infection
- Zika virus infection
- See also “Yellow fever”
- Babesiosis
- Campylobacteriosis
- Chagas disease
- Chancroid
- Coccidioidomycosis
- Cryptosporidiosis
- Cyclosporiasis
- Cysticercosis
- Echinococcosis
- Ehrlichiosis
- Giardiasis
- Gonorrhea
- Granuloma inguinale
- Herpes simplex, neonatal and genital (initial infection only)
- (Providers)
- Histoplasmosis
- Human immunodeficiency virus (HIV) infection
- Human prion disease
- Lyme disease
- Lymphogranuloma venereum
- Malaria
- Relapsing fever (borreliosis)
- Rickettsia infection
- Serious adverse reactions to immunizations
- Syphilis
- Taeniasis
- Tetanus
- Tick paralysis
- Trichinosis Typhus
- Varicella-associated death
Notifiable Within 30 Business Days
- Cancer (See chapter 246-102 WAC) wscr@doh.wa.gov
- Facilities Only
- Gunshot wounds (nonfatal)
- For birth defects listed above, call 360-236-3533
- Notifiable to L&I - 360-902-5669
- Asthma, occupational Hypersensitivity pneumonitis, occupational
- Silicosis
Rapid Screening Tests
Providers and facilities performing blood lead level RST shall report as a laboratory and comply with the requirements of WAC 246-101-201 through 246-101-230.
- Blood lead level**
- RST results (See WAC 246-101-200)
- Coronavirus infection (severe communicable)
- Novel coronavirus (COVID-19)
- RST results (See WAC 246-101-200)
- Novel coronavirus (COVID-19)
- Hepatitis C (acute infection)
- RST results (See WAC 246-101-200)
- Hepatitis C (chronic infection)
- RST results (See WAC 246-101-200)
- Human immunodeficiency virus (HIV) infection
- RST results (See WAC 246-101-200)
Notifiable Conditions
Laboratories
Notifiable to the local health jurisdiction (LHJ) of the patient’s residence unless otherwise designated.
Download the Report Reference STI Reporting FormLegend
Bacteria
-
Rickettsia species including, but not limited to:
- Rickettsia rickettsii
- Rickettsia africae
- Rickettsia typhi
- Rickettsia parkeri
- Rickettsia philipii
Viruses
Parasites
Fungi
Other
Notifiable to Department of Health (DOH)
* Notify DOH (except King County where this is notifiable to LHJ)
Notifiable Conditions Reporting Forms
Animal Bite Reporting Form for Suspected Rabies Exposure
If wishing to complete the form by hand, download, print and fax the Animal Bite Reporting Form for Suspected Rabies Exposure to 509.397.6239.
General Communicable Disease Reporting Form
If wishing to complete the form by hand, download, print and fax the General Communicable Disease Reporting Form to 509.397.6239.
Sexually Transmitted Infections Reporting Form
If wishing to complete the form by hand, download, print and fax the Confidential Sexually Transmitted Infection Case Reporting Form to 509.397.6239.
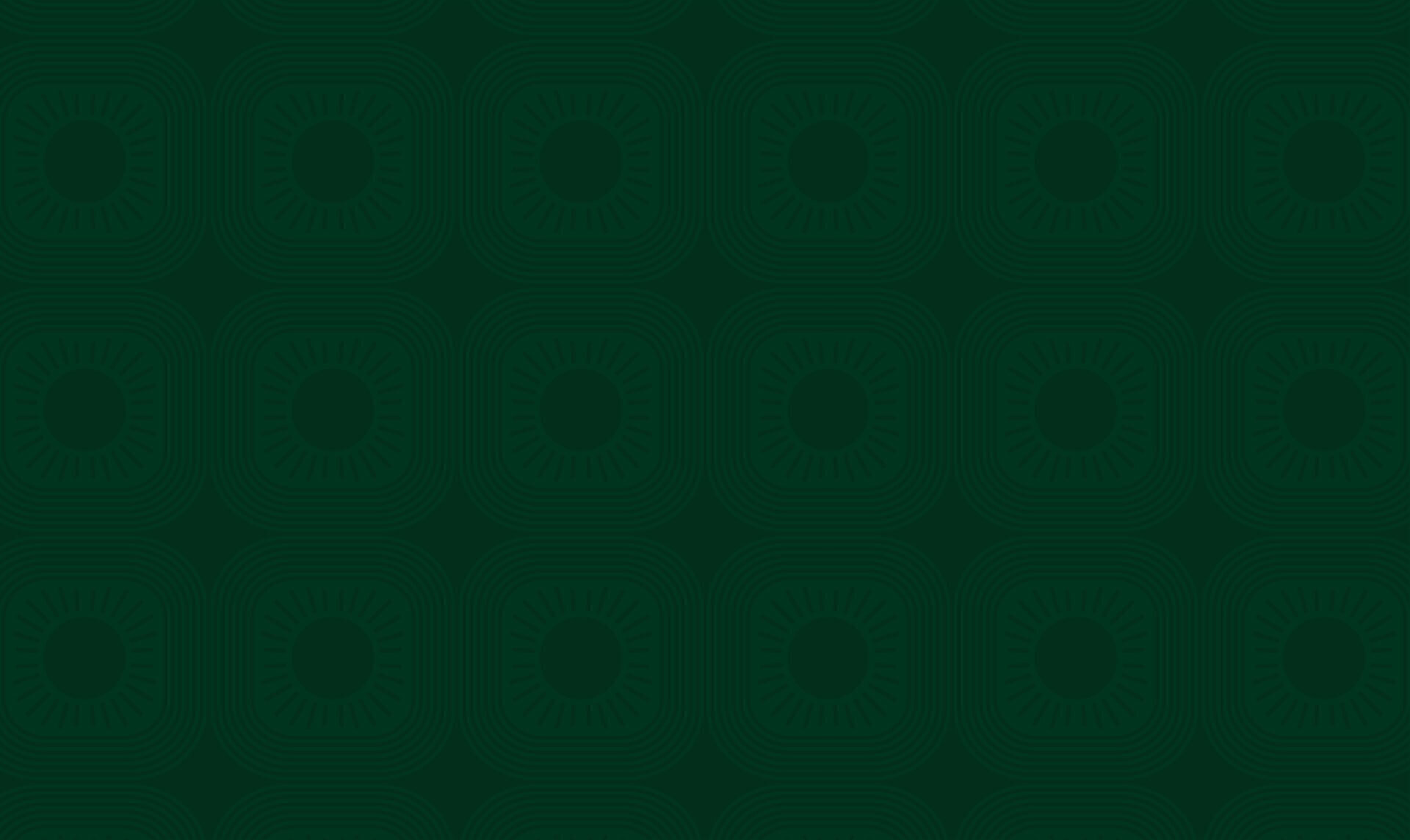
Measles Guidance
Actions Requested of Health Care Providers
Maintain a high index of suspicion for measles to identify those infected.
Please consider measles in patients presenting with fever, rash, and any of the following: cough, runny nose, or red, watery eyes—especially if they have had contact with someone known to have measles or symptoms consistent with measles.
If you suspect measles:
1. Test
Early testing helps confirm diagnosis and guide public health actions. NP swab for PCR is the most sensitive test and preferred in the prodromal period but is most accurate 0-5 days after rash onset. If it has been between 72 hours and 10 days since rash onset, it is recommended to collect an NP swab AND urine for PCR.
2. Initiate isolation promptly
Do not wait for lab results before taking action. Measles is highly contagious, so implement airborne precautions immediately. CDC provides detailed guidance for measles management and infection control in healthcare settings.
3. Exclude
Advise the patient to stay home from work, school, or childcare until at least 4 days after the onset of the rash.
4. Educate
Consider using WCPH's Measles Fact Sheet to help educate patients and families about measles symptoms, transmission, and isolation recommendations.
5. Ask about close contacts
Identify and assess close contacts for immunity.
Offer post-exposure prophylaxis (MMR vaccine within 72 hours or immune globulin within 6 days) to susceptible individuals.
Infants under 12 months, pregnant people without evidence of immunity, and immunocompromised contacts are especially high priority.
Advise all contacts to monitor for symptoms for 21 days after exposure and CALL FIRST before coming in to the office.
6. Report the illness to Whitman County Public Health immediately
We will conduct an interview with the patient to confirm isolation, assess exposure risk, and assist in determining recommendations for post-exposure prophylaxis and exclusion.
7. Prioritize vaccination
Ensure children and adults are up to date on MMR vaccination according to national immunization guidelines.
Measles Assessment Checklist for Providers
DOH Guidance
Adult Measles Vaccine Recommendations
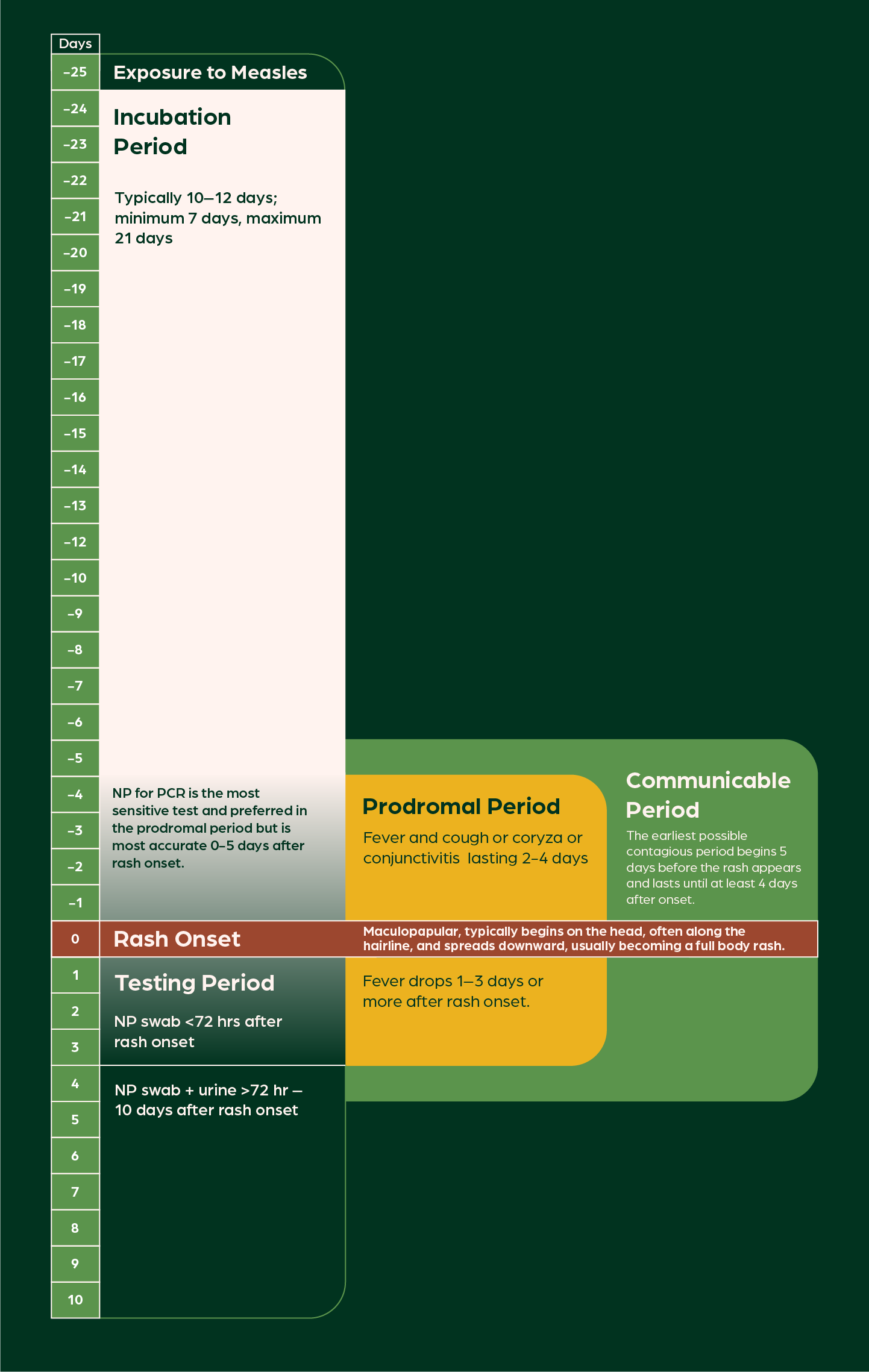
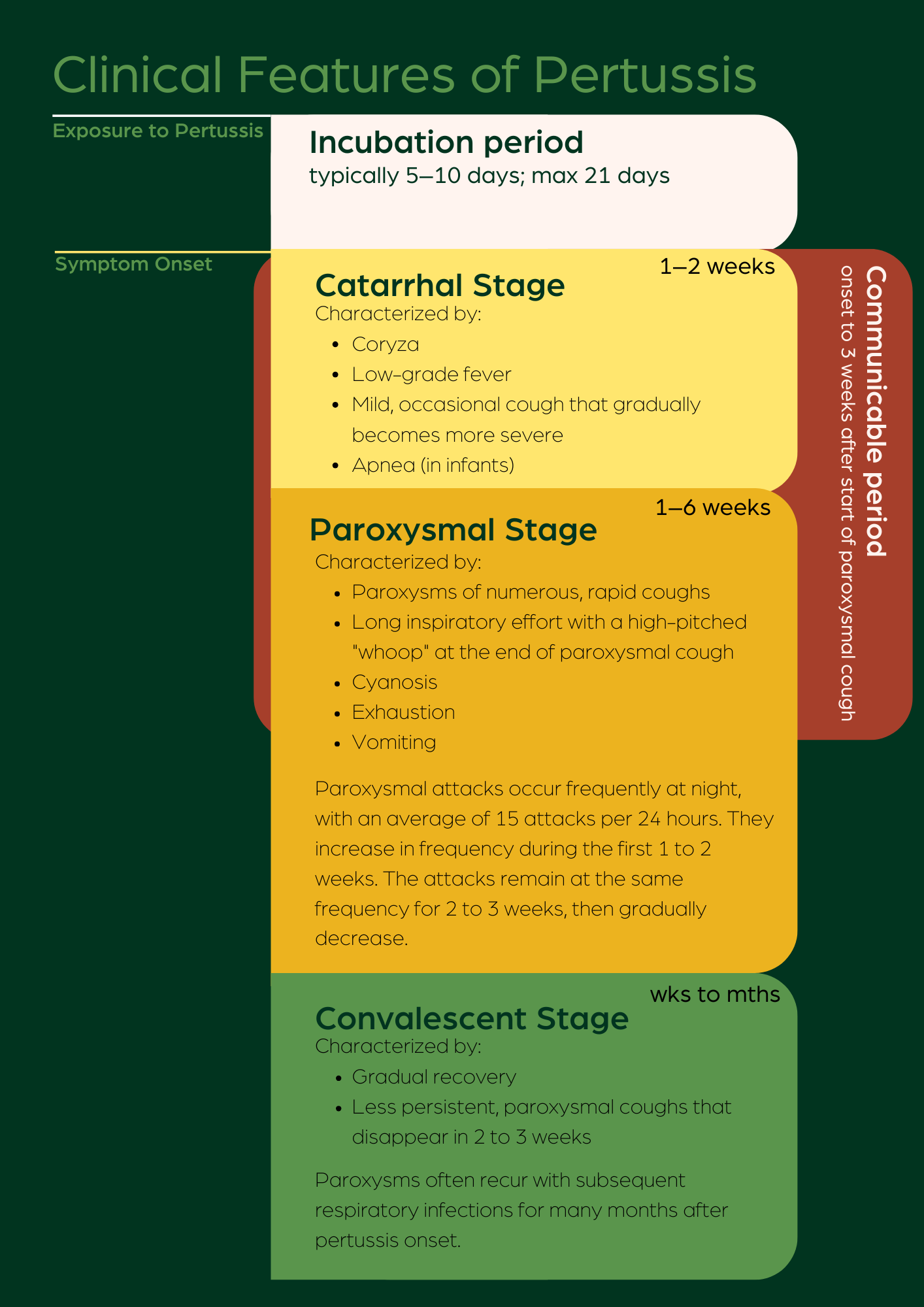
Pertussis Guidance
Actions Requested of Health Care Providers
Maintain a high index of suspicion for pertussis to identify those infected.
Please also consider pertussis in a respiratory illness of any duration in patients who have had contact with someone known to have had pertussis or symptoms consistent with pertussis.
If you suspect pertussis:
1. Test
Collect a nasopharyngeal (NP) swab for Bordetella pertussis PCR or culture. PCR is the most sensitive and fastest diagnostic test and is widely available at commercial laboratories.
2. Initiate treatment promptly
Do not delay treatment while awaiting results. CDC provides detailed treatment guidance.
3. Exclude
Tell the patient to stay home from work, school, or childcare.
Advise them that they are considered contagious until they have completed 5 full days of appropriate antibiotics.
4. Educate
Consider using WCPH's Pertussis Fact Sheet to help educate patients about pertussis and isolation recommendations.
5. Ask about close contacts
Consider preventive antibiotics for the entire household AND any close contact who meets “High Risk” criteria.
- Infants under one year old
- Pregnant people, especially those in the third trimester.
- People who have a chronic respiratory illness.
- Family members or caregivers of infants or pregnant women.
Symptomatic close contacts should be treated as soon as possible and
excluded from public activities until they have completed 5 days of
antibiotics.
Asymptomatic close contacts and those taking preventive
antibiotics do not need to be excluded from activities unless they
develop symptoms.
Advise family members and close contacts who are not taking preventive antibiotics to return promptly if they develop symptoms within the next 21 days.
6. Report the illness to Whitman County Public Health within 24 hours.
We will conduct an interview with the patient to confirm isolation and treatment. We can also assist in determining recommendations for prophylaxis and exclusion.
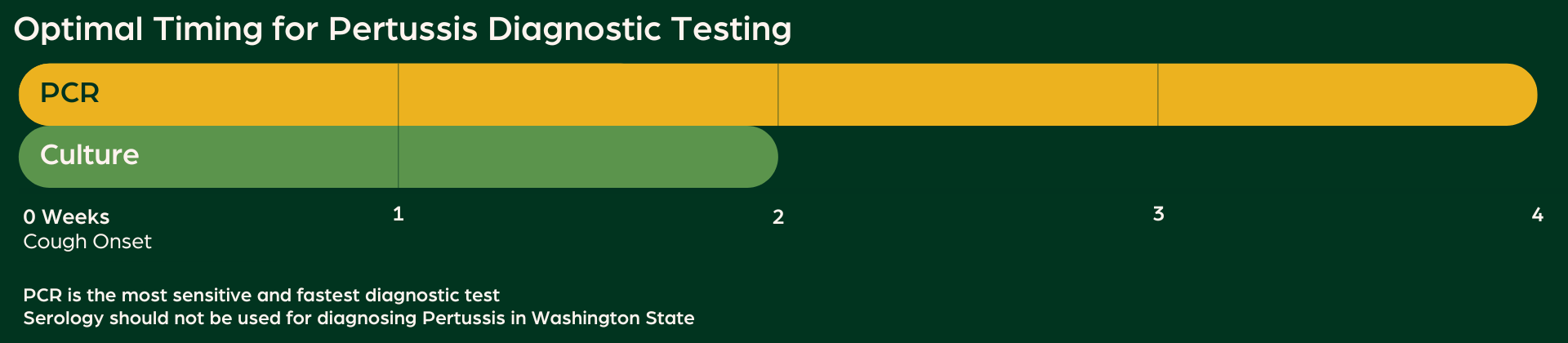
7. Prioritize vaccination
Assure children and adults are up to date on pertussis-containing vaccines according to national immunization guidelines.
COVID-19 Guidance
Vaccination Guidance
DOH COVID-19 Vaccine Guidance
COVID-19 Vaccine Schedule for Healthcare Providers
Provider Alerts
For general disease prevention updates for all of Whitman County, click on the "Disease Prevention Updates" button below.
Environmental Containments
Feb 9, 2026
Fatal Case of Histoplasmosis Suspected to be Acquired in Whitman County

Illness from Animal
Jan 9, 2026
Potential for Travel-Associated New World Screwworm Myiasis

Bacteria
Jan 1, 2026
Provisional Notification & Submission of Specimens for Invasive Haemophilus Influenzae Disease

Animal-To-Human
Jan 30, 2026
Brief Guidance for Healthcare Personnel Exposed to a Human HPAI Case
Provider & Community Health Alerts
Be the First to Know
From advisories to urgent alerts, get accurate public health updates that help keep you and your patients safe.